Neonatal Intensive Care Unit

The Neonatal Intensive Care Unit (NICU) at the Children's Hospital in Newcastle provides highly specialised, family-centred care for sick and premature newborns.
The arrival of a newborn baby is a very exciting time for parents and families. Our team of dedicated, caring and compassionate medical professionals recognise that having your baby admitted to NICU can also be a difficult time. Our first priority is taking care of your baby and family.
Tour the Neonatal Intensive Care Unit
Your baby's birth and arrival in NICU
When your baby needs support at birth, the NICU team will be there to help. There will be specialised care for your baby in your delivery room. The first minutes are vitally important, and can seem busy. We know that the first moments of touch and sound are cherished by parents and we will make every effort for you to hold your baby before transfer to NICU.
The first hour in NICU can be busy as we get your baby settled in. If you are unable to be there, we will keep you informed about your baby’s progress.
Temperature
Maintaining the right body temperature is important for your baby’s well-being. In the delivery room, tiny babies are wrapped first in a type of cling wrap. Bigger babies are dried and wrapped in a blanket.
In NICU, some babies need a humidicrib to provide warmth and sometimes humidity, this bed also lets us see your baby. If your baby is in a humidicrib we will show you how to care for your baby.

Lungs and breathing
Breathing difficulties (Respiratory distress) are important and frequent signs in NICU. Your baby’s lungs might be stiff or small, have too much fluid or infection. Preterm babies can require help to ensure regular breathing even when lungs are normal. Breathing support is given with CPAP or a ventilator, and extra oxygen if needed. This support will gently assist your baby’s own breathing. A chest X-ray is done in NICU when needed.

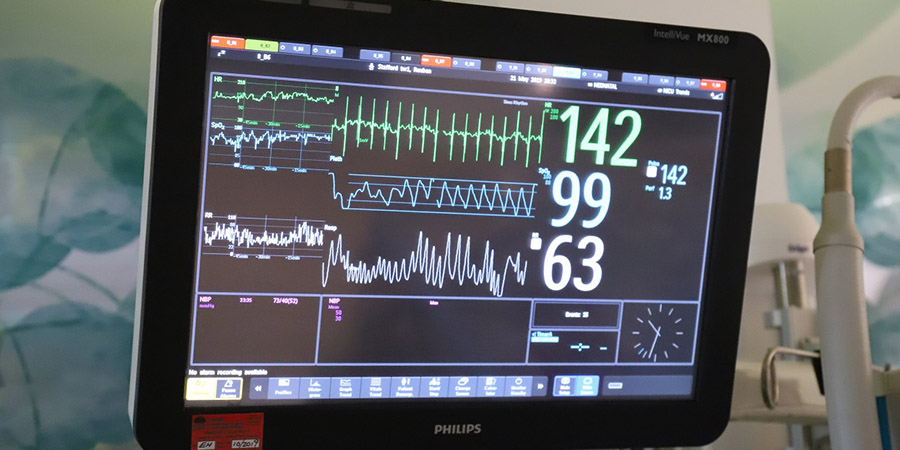
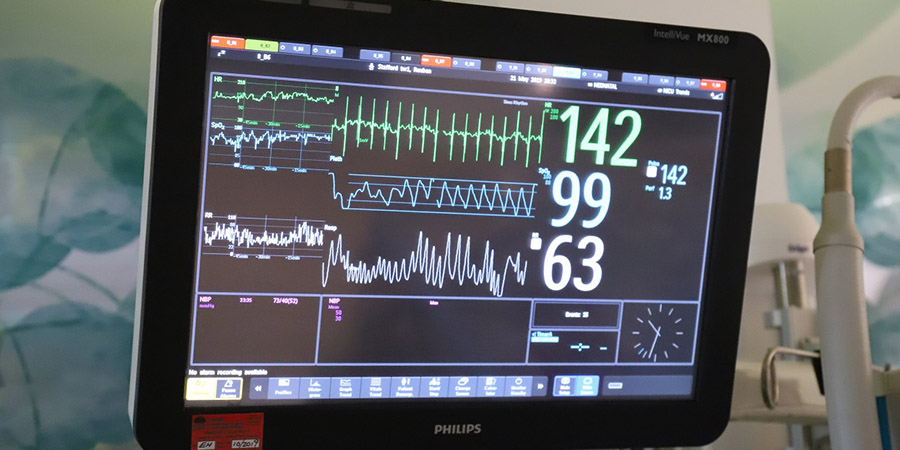
Observation
Your baby’s heartbeat, breathing, and oxygen level are observed continuously on a monitor. Sticky leads are placed on the chest, and stretchy tape holds leads on the hand or foot. Blood pressure is also measured. All this monitoring together shows how the heart and lungs are working. If an alarm rings on this monitor, do not panic the staff caring for your baby know how to respond and will explain what is occurring to you.
Fluid and nutrition
Intravenous cannula’s (lines in veins) are used for giving fluids and nutrition, for taking blood tests, and for continuous monitoring. Breast milk is the best food for all babies, especially preterm babies. Support, guidance, and equipment will be available for you to express. Then when your baby is ready, your breast milk is ready.
Watch: A parents journey through NICU
NICU for parents
While your baby is in NICU, you belong here too. You are always welcome. The bedside nurse will support and guide you in the care of your baby, they will introduce you to the bed space your baby is being cared for in and the facilities available in this region. During times of procedures or increased activity, you will be shown to the family waiting area.
There are visiting restrictions on other family members and friends. Visiting is with your written permission only, and your bedside nurse will record if you give permission for others to visit your baby. AS OF 13 MARCH 2022, VISITING RESTRICTIONS WILL BE IN PLACE DURING THE COVID-19 PANDEMIC - NICU visiting restrictions during COVID-19.
There is a quiet time in NICU from 12pm to 3pm, during which parents may sit quietly, but visitors leave.
Your baby’s area can have no more than two parents at a time.
Each bed space has a nursing side and a family side. Generally the right side of each bed space has family facilities. These include a recliner chair, sitting chair, breast pump, milk fridge, milk warmer and patient care board. The fridge is for you to store your baby’s milk in. Please ask the nursing staff how to use this equipment and how long your milk can remain in the fridge.
For the safety of your baby
- Please do not bring food or hot drinks into NICU (water is permitted)
- Please use the cots to move your baby around the NICU and between wards
- Please respect the privacy of other babies and families in the NICU/SCN
- Please be aware that smoking is harmful, if you do smoke, chemicals from cigarettes may stick to your skin/hair/hands and can be detected in your baby. The best way to prevent this is stop smoking and ask our staff for assistance. If you choose to smoke please wash your hands well and wear an over garment when smoking that can be removed when visiting your baby.
Infection prevention and hand washing
Babies are at risk of infection. Please ensure you and your visitors are aware of the infection prevention measures (Five Moments of Hand Hygiene) to reduce the risk of transmitting an illness to your baby (refer to our House Rules). Gel is placed at every bed-side; this should be used before and after you or anyone touches your baby. A way to remember is GEL-BABY-GEL. Please remember mobile phones and cameras do carry infection and need to be wiped down if used in the NICU environment. If you or one of your family members is sick, please do not visit without having a discussion with nursing staff. This is to prevent any babies in the NICU getting sick.
You and your baby
Bonding and attachment
Even though your baby’s medical needs require that he or she be cared for in the hospital’s neonatal unit, you are still the most important person in your baby’s life. Your baby knew your voice even before birth and needs your special touch.
We encourage you to talk to, read to, touch and caress your baby as much as his or her medical condition will allow. The human touch, especially, that of a parent, has as much to do with getting well as does all of the medical technology and expertise.
Kangaroo cuddles
This provides skin to skin contact between baby and parent, so your baby can experience the feeling of warmth and comfort associated with this contact. There are many short-term and long-term benefits of skin to skin care for instance a kangaroo cuddle with you is a perfect way to help control your baby’s temperature so we encourage and support parents to do this whenever possible. We will help position your baby safely for Kangaroo cuddles and will always be available should you need support.
Patient care boards
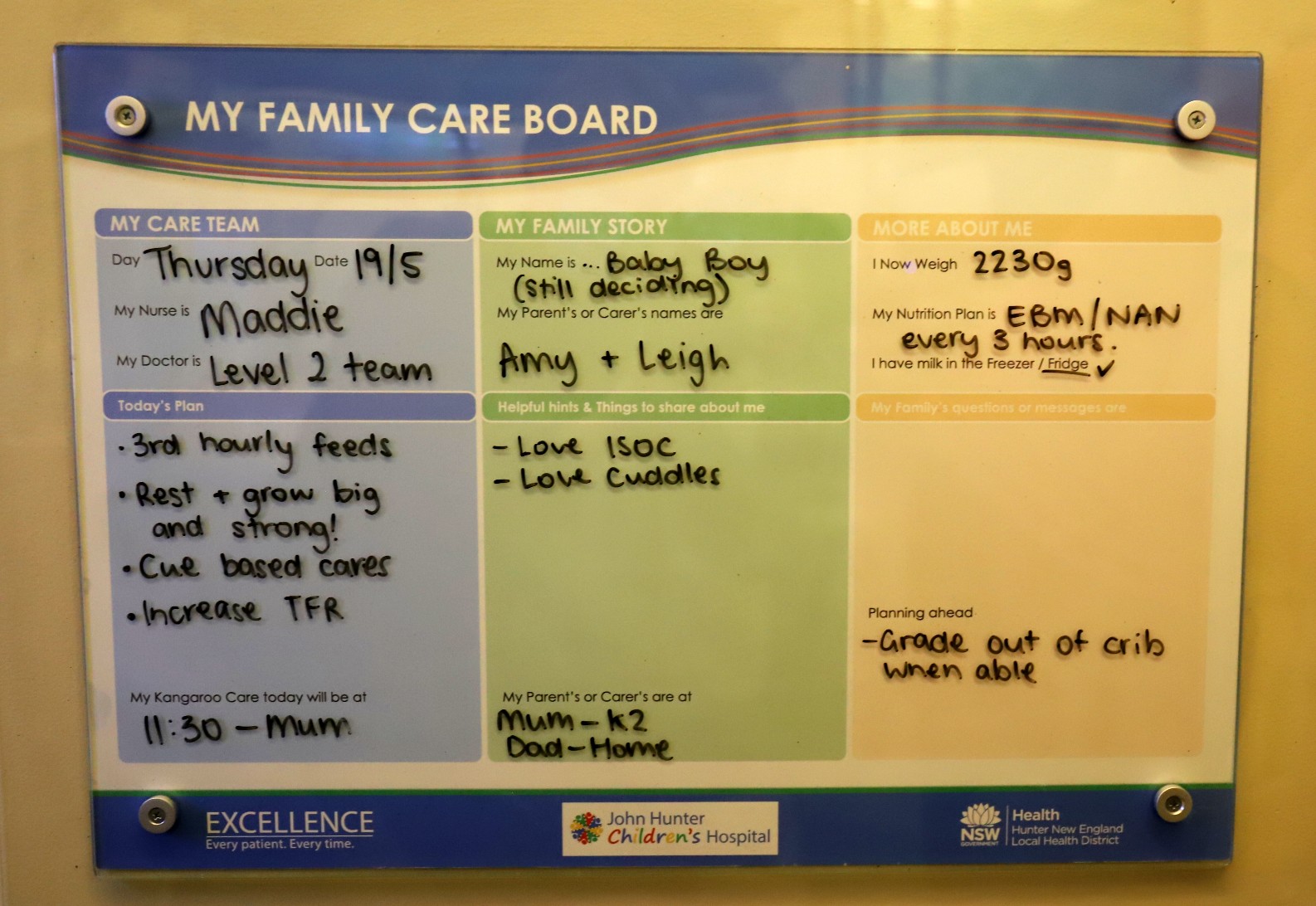
These are a communication tool to help individualise patient care for your baby. It also makes it easier for the health care team and you as a parent, family and/or carer to plan and understand the care that is provided for your baby on a daily basis. Both you and the staff can write on the boards.
Photography
Flash photography will not harm your baby, so feel free to take as many photos as you wish with your own camera. You are welcome to bring in your own video camera to take videos of your baby. Please remember to gel hands after touching any equipment before you then touch your baby.

Clothing
We provide clothes for your baby but you are welcome to bring clothes in if you wish. We will do our best to ensure these will be placed in a plastic bag when soiled for you to take home and wash. Please label any clothes or blankets.
NICView
NicView is a web camera specifically designed for use in the NICU. NicView allows you to see your baby in NICU whenever you wish when you are not in the hospital.

Bath
In the NICU you will learn how to care for your baby, including giving them a bath from time to time. This may be a gentle sponge bath for babies in cribs or a big bath for babies who are in a cot. The nurses will be there to help you along the way, so talk to them about your baby’s bath routine.
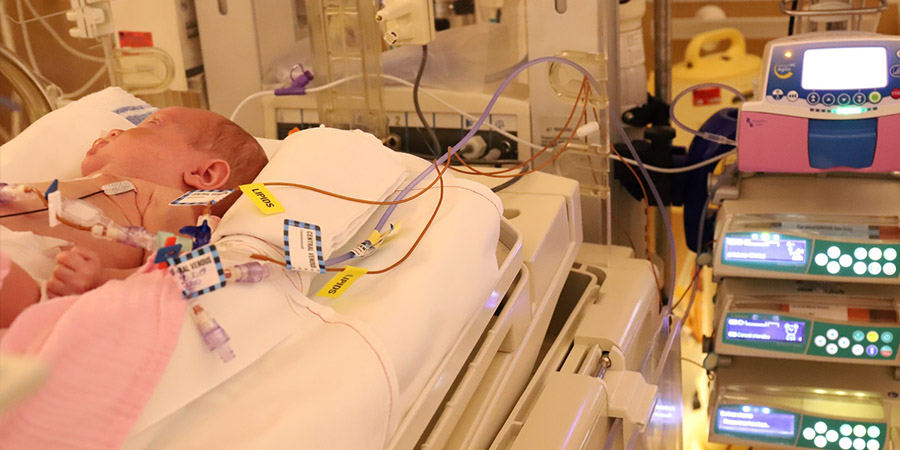
Medical equipment used in NICU
Initially, seeing all of the medical equipment used for your baby can be overwhelming. The noises, beeps, clicks, alarms and flashes of machines will seem strange at first, but over time you will become familiar with the equipment and learn how each machine is helping your baby. The nursery staff will be happy to explain any equipment to you.
Following is a brief list of medical equipment you may see in the unit.
Omnibed (Giraffe bed)/Incubator/Humidicrib/Isolette
This is an enclosed bed that provides a warm, clean, and controlled environment for your baby.

Open care bed
This is an open bed with special overhead heater.
These beds keep your baby warm whilst permitting easy access for parents, nursing and medical staff from all sides.

Monitor
This is a machine that displays your baby’s heart rate, heart beat pattern, blood pressure, breathing rate, breathing pattern and level of oxygen in the body.
Pulse Oximeter
A small device that monitors oxygen levels in the baby’s blood. It is usually attached to your baby’s hand or foot and secured with a stretchy tape.

Temperature probe
This monitors your baby’s skin temperature to ensure your baby’s temperature stays within the normal range.
Gastric tube
A soft tube inserted through the nose or mouth into the stomach. This tube can be used to feed your baby and administer medications.

Infusion pump
 This device slowly and continuously administers fluids and medications to your baby at a desired rate through intravenous lines.
This device slowly and continuously administers fluids and medications to your baby at a desired rate through intravenous lines.
Nasal cannula
A method of giving oxygen or mixture of oxygen and air to your baby through small, flexible, plastic tubes placed in his/her nostrils.

CPAP (Continuous Positive Airway Pressure)
This a method used to help support your baby’s breathing. The CPAP is delivered by two short plastic tubes (prongs) in the nostrils.

Ventilator
This machine is used to assist your baby’s breathing when (s)he cannot breathe well enough on his/her own.

Feeding your baby
We encourage all mothers to provide breast milk for their baby. Breast milk is the best tolerated food and helps protect against diseases. Even if your baby is too sick or premature to suck we encourage expressing your milk as soon as possible. The staff of the NICU and postnatal ward will support you in your choice of breast or formula feeding.
When your baby is ready to start milk feeds she/he may have a tube passed through his/her mouth or nose directly into the stomach, to feed milk in small amounts. This will be increased as your baby digests the milk and grows.
The neonatologist/nursing staff will let you know when your baby is ready to start breast or bottle feeds. To make sure your baby doesn’t get too tired, sucking feeds may be offered only once or twice a day at first.
Breastfeeding
If you plan to breastfeed it is important to establish your milk supply by hand expressing every 3 to 4 hours and switching to expressing by pump once your milk supply is established. This may seem like hard work but it is worth the effort and your baby will benefit from the breast milk.
It is normal to express small volumes of breast milk at first but this will increase over time. To help to increase your supply, drink enough water, eat a good, healthy diet and make sure you have plenty of rest. We recommend reducing your intake of caffeine and stopping cigarette smoking. If you need assistance to stop smoking the staff in NICU can help you.
The NICU has a Breast feeding/Expressing Room available for all expressing mothers and a breast pump and milk warmer by each bed space. This room provides a quiet, private space to use the electric breast pumps that are available. To ensure privacy this room is for mothers only. Some mothers may prefer to express near their baby’s bed space. Breast pump kits are available on loan and can be obtained from the nurse caring for your baby. The nurse or Lactation Consultant can help you with the setting up and use of the equipment. They can answer any questions you may have.
Store your breast milk in plastic cups with lids. These must be BPA free and must be sterilised before use. Use of Milton solution, steam steriliser or microwave steriliser is recommended. The nurse caring for your baby will supply you with labels for use with these containers. These labels have your baby’s name and medical identification number printed on them. Write the date and time of expressing and place in either the fridge or freezer in your baby’s own labelled tray.
Information sheets are available on where to purchase containers and hire breast pumps or purchase pump kits for use at home. In addition, information sheets outlining sterilising equipment, handling, storing and transport of breast milk are also available.

Tube feeding
Tube feeding is performed via a gastric tube, which is inserted through the nose or mouth into the stomach. This tube can be used to feed your baby and administer medications.

Routine tests and procedures for your baby
All babies weighing less than 1500gms and/or less than 32 weeks gestation at birth will routinely have the following tests/procedures.
Head ultrasound
The head ultrasound is able to detects any changes and is done during the nursery stay. This is a painless procedure, similar to the ultrasound you may have had during pregnancy. The probe scans through the soft spot on the top of your baby’s head (fontanelle). Babies usually sleep through this procedure. The ultrasound is usually performed within the first 48 hours of life and repeated at one week of age and again at one month of age. The results will be discussed with you by the doctor when the results are available.

Eye examinations
Small babies will have an eye examination to screen for “eye disease of prematurity” called Retinopathy of Prematurity. This will be carried out in babies born 30 weeks gestation or less, when your baby is 28 days old and approximately 32 weeks corrected age. You will receive more information when your baby’s eye check is due. Some babies will need an ophthalmology review for other reasons.
Newborn Screening Test (NBST)
This is a blood test for babies in the first 24 - 48 hours. If your baby weighs less than 1500 grams at birth a repeat NBST will be attended at 28 days of age. You will be given information about this test by the bedside nurse, and asked for your consent.
Universal Hearing Screening (SWISH)
All babies are offered a hearing screen closer to term. This is also available at your local hospital.
Saturation Screening for Congenital Heart Disease
All babies have hand and foot oxygen levels measured with a small probe placed on the baby’s hand and foot before going home. It takes less than 5 minutes. 99% of baby’s pass this test, if your baby has to be re-tested, the result will be discussed with you.

Immunisation
All infants requiring immunisation will be identified and given appropriate immunisation in a timely, safe and effective way, based on the National Immunisation Program Schedule. Parents will be given information regarding immunisation and have any questions answered to allow an informed decision to be made.
Cardiac Ultrasound
A cardiac ultrasound, also known as an echocardiogram, is an ultrasound study of your baby's heart. It looks at heart structure, blood flow and muscle function. Some babies need this to screen for or diagnose problems with their heart or major blood vessels. You may also hear the words echo or cardiac echo for this test.

Blood tests
Babies in the NICU need frequent exams and monitoring as part of their care. At times this includes testing of the blood as they help to monitor your baby’s condition and to identify potential problems. Common tests include, testing for anaemia (low red blood cells), electrolyte and mineral levels, blood sugar levels or testing for infection. The tests are more commonly attended by collecting blood from the baby’s vein or heel.

Phototherapy
Facilities for parents
A number of services and facilities exist within the NICU and on the hospital campus for your convenience while your baby is in NICU.
Ronald McDonald Family Room
Situated within the NICU, the Ronald McDonald Family Room is available for parents to and take some ‘time out’. There is a lounge area, children’s play space as well as tea and coffee making facilities. Ask your social worker for opening hours. Basic meal provision may be available and the room is available for all parents, local and from regional areas of NSW. In addition there is a Family Room on Ward J1 that also has laundry facilities.

Lockers
Lockers are available for families to store their belongings, there is a locker by each bed space, or at the entrance to the NICU. The lockers by bed spaces are not secure, however those near the entrance can be secured by lock and key, this requires a $2 coin, which is refundable on departure.

Accommodation
We have limited short stay accommodation available for emergency situations only. NICU Social Workers can discuss this with families who may require it.

Places to eat
The hospital cafeteria “The Cosy Kooka” on Level 1 (adjacent to H1) is available to parents and visitors for meals at a lower cost. “Café Grab ‘n Go” and the Food Hall in the Royal Newcastle Centre are available for refreshments on Level 2 in the hospital foyers.
Due to safety issues hot drinks or food are not allowed in the nursery. There is a cold water fountain for your use in the entry hall of the nursery.
Parking
Parking is available 24 hours a day.
Public rates and concession rates apply:
Public rates
| 0- 20 mins | Free |
| 20 mins- 1 hour | $2.50 |
| 2 hours- 3 hours | $5.00 |
| 3+ hours | $10.00 |
Concessions only rates
| 0- 3 hours | Free |
| Between 3 and 24 hours | $5.60 |
| 3 day ticket | $11.30 |
| 7 day ticket | $22.60 |
Toilets
Toilets are available in the entrance to NICU. There is a baby change facility and shower facility in this area.
ATM
The Newcastle Permanent has one ATM located within the John Hunter main entrance.
Chapel
A chapel is located on Level 2, adjacent to the John Hunter main entrance.
Free WiFi
The Children’s Hospital has free guest wifi available. To access in NICU, search wifi on your device and select ‘_NSW_Health_Guest_Wifi_HNEH’.
Parent education
NICU babies need special care at home too, and we aim to build your skills in your approach to your child’s development. You can attend sessions more than once – practice makes perfect – and start attendance as soon as you’re ready. Check the electronic screen near the parent toilets for times and information.
Discharge preparation
NICU research
Many thousands of NICU babies have been part of neonatal research, which has helped to improve the care provided today. Your baby’s participation will continue this improvement, helping future babies.
Before research studies begin they pass through strict checks by committees to ensure that they are safe. You are always welcome to ask any questions regarding the potential benefits, risks or post-trial information of the research study.
Remember that ultimately the decision to participate in research or not is yours, and we will respect your decision. You may also withdraw your baby from a study if you wish to at any time. Your decision of not participating in the research or withdrawing from a study will not affect the quality of clinical care provided.
Neonatal Intensive Care Units Survey (NICUS)
NICUS (Neonatal Intensive Care Units) is a program put in place to ensure we provide the highest possible standards of care for sick and/or premature babies in NSW & ACT.
In an effort to improve patient care nationally information is gathered to give a complete picture of the pregnancy, treatment and progress of your baby in the Neonatal Intensive Care Unit and Special Care Units. For such a system to be accurate and reliable it is vital that every eligible baby in NSW and ACT is included. With your permission, your baby will be enrolled when meeting NICUS criteria. Please feel free to ask the nurse Team Leader for any information about NICUS.
Transfer from the nursery
When your baby was admitted to the NICU you may have been transferred from another hospital.
Once your baby is getting better and big enough, we will organise transfer back to your referring hospital so you and your baby can be closer to home. You will be given an information pamphlet about your referral hospital.
Going home
Your baby is ready to go home from the nursery when your baby;
1. Is 35 weeks corrected gestation or more,
2. Is feeding and growing well – breast, bottle or sometimes tube feeding,
3. Is maintaining temperature.
Follow up
Babies born less than 1500 grams or less than 32 weeks gestation at birth, or have complex issues will be followed up in the Neonatal Growth and Development Clinic shortly after discharge and at 3, 6, 9 months corrected age by one of our Neonatologists, Liaison CNC and a Physiotherapist.
At 12 months and 24 months corrected age some babies will be given a formal Developmental Assessment. This assessment involves being seen by our Developmental Neonatologist or an Occupational Therapist who will run through a series of tasks with your baby to assess how their development is progressing. We will contact you close to the time the assessment is due to arrange an appointment. If you change your address or phone number after discharge from this nursery, please contact us on 02 49214362 with your new details.
Blue Book
This is your baby’s personal health record and will remain with your baby during admission to hospital. Once your baby goes home, we recommend that you keep this book in a safe place and take to any clinic or doctors appointments.
Support Services
- Neonatal Intensive Care Unit - 24 hours a day – ask for the Team Leader
- Australian Breastfeeding Association – 1800 686 268 (1800 mum2mum)
- Your local Child and Family Health Nurse
- NSW Health Line – 1800 022 22
Ask the nursing staff for more information on these services.
People in NICU
There are many staff members working in the NICU. If you have any questions please ask the nurse looking after your baby, they can help put you in contact with the correct person.
Dr Larissa Korostenski- Head of Newborn Services

Natalie Butchard- Manager, Newborn services
Neonatologists

Dr Paul CravenNeonatologist

Dr Rebecca GloverNeonatologist

Dr Koert De Waal

Dr Anil LakkundiNeonatologist

Dr Joanne McIntoshNeonatologist

Dr Nilkant PhadNeo
natologist
Nursing managementNurse Unit Manager

Kristy ChesworthNurse Unit Manager

Megan YoungNurse Unit Manage
Room phone numbers
NICU room phone numbers
| Room 1 | 49236722 or 49236726 |
| Room 2 | 49236627 or 49236628 |
| Room 3 | 49236629 or 49236631 |
| Room 4 | 49236665 or 49236666 |
| Room 5 | 49213375 |
| Room 6 | 49213496 or 49223347 |
| Room 7 | 49236667 |
Special Care Unit phone numbers
| Room 8 | 49236310 or 49236311 or 49236312 |
| Room 9 | 49236307 or 49236308 or 49236309 |
| Room 10 | 49236304 or 49236305 or 49236306 |
| Room 11 | 49236301 or 49236302 or 49236303 |
Compliments and concerns
If you wish to pass on a compliment or have any concerns please speak to any of the following staff members:
- The nurse or doctor caring for your baby,
- The nurse in-charge,
- The nursing unit manager, or
- The social worker.
At John Hunter Children’s Hospital you are a part of the team and our goal is to include you in the planning for your baby’s treatment and keep you up to date with their progress. We take your concerns very seriously and are happy to discuss them with you, or direct you to the people who can best help answer your questions.
REACH- Patient and Family Escalation Information
If you are worried about a recent change in your baby, REACH out.
This fact sheet provides families and carers with information about the program and how you can reach out to our clinicians if you are concerned about your child's condition.
Please call:
From bedside: 13620
From mobile: 4921 3620